Getting into anaesthetics training is very competitive – the first step to have a chance is to get a great score in the Multi-Specialty Recruitment Assessment…
Read MoreThe MRCGP AKT exam is a challenging exam, testing applied knowledge relevant to UK general practice. In this article, Dr Mahibur Rahman discusses some key tips…
Read MoreWorking as a junior doctor comes with lots of challenges – including balancing a busy rota with home life whilst also preparing for exams and assessments.…
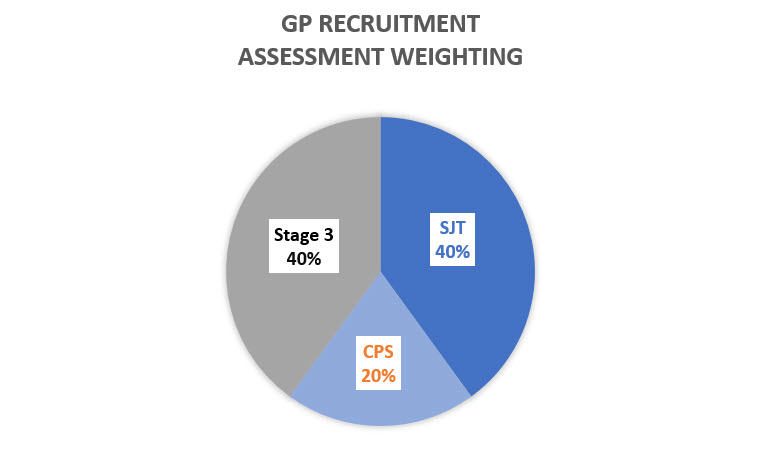
Read MoreThe weighting of the different assessments as part of the GP recruitment process have changed for 2018/2019 recruitment. This article covers how the different parts are…
Read MoreStarting your first job as a qualified doctor or in a new hospital / system can be exciting, but it can also be scary and comes…
Read MoreOnce you have finished training, there are many career options open to you. Some are obvious – become a principal in a partnership, take a salaried…
Read MoreWorkplace based assessment (WPBA) is one of the 3 components of the MRCGP exam. In this article, Dr Mahibur Rahman provides an overview of WPBA –…
Read MoreTalking to the families of your patients can be one of the more difficult parts of your life as a doctor, but you can make it…
Read MoreWhen starting GPST, if you have to move house (i.e. your new job is in a different area), there are certain expenses that you can claim. …
Read MoreThe MRCGP CSA is a challenging exam, acting as an exit exam for GP training in the UK. In this article, Dr Mahibur Rahman discusses some…
Read More